The Medicare Advantage Strategy
Ellsworth Consulting develops and executes strategies for provider clients to navigate the evolving Medicare Advantage landscape.
We work with clients to improve MA margin yields, limit exposure to MA growth and/or reduce the number of contracted MA plans.
Medicare Advantage, also known as Part C, is a comprehensive alternative to traditional Medicare, offering seniors an all-in-one healthcare plan. With increased enrollment, it has become a key focus for both payers and providers. However, the landscape is facing a series of significant challenges that are reshaping how organizations operate within this space.
As pressures continue to mount, a proactive approach is essential for ensuring sustainable success in this changing environment.
Providers face their own set of pressing challenges within the Medicare Advantage ecosystem. According to S&P Global in a recent report, “As of 2023, more than half of the Medicare population is enrolled in a MA plan, and payments to these plans now exceed traditional Medicare.” With Medicare Advantage now covering the majority of seniors, providers are grappling with yields of only 80%, largely driven by aggressive down coding and an increase in claim denials.
Hospitals need to acknowledge the reimbursement problem and proactively address their relationships with payers head-on.
For payers, the current environment is akin to a perfect storm. Competition is intensifying as more insurers enter the Medicare Advantage market, leading to margin compression. Additionally, the CMS has announced rate cuts for 2025, further straining profitability.
V28 Risk Adjustment changes and stars reductions for many plans also create significant financial pressure. As a result, benefit cuts and premium increases are likely on the horizon as payers work to navigate these difficulties.
These lower reimbursement rates, coupled with slow pay, no pay, and low pay policies from payers, are squeezing provider margins to unsustainable levels. As a result, Medicare Advantage reimbursements are approaching those of Medicaid, creating an alarming financial strain for many healthcare organizations.
Moreover, the excessive administrative burden of navigating complex claims processes, coupled with lengthy delays and appeals, is adding significant operational strain to providers who are already working to manage high patient volumes.
Providers need a clear strategy to adapt and thrive. From enhancing patient engagement to optimizing reimbursement processes, we collaborate with providers to execute strategies that ensure financial viability and operational efficiency.
Contact us today to see how we can help.
Recent Client Medicare Advantage Strategy Success Story
-

Changes coming to Medicare Advantage plans accepted by Blessing Health
QUINCY — Blessing Health System has announced changes will be coming to which Medicare Advantage plans the company accepts.
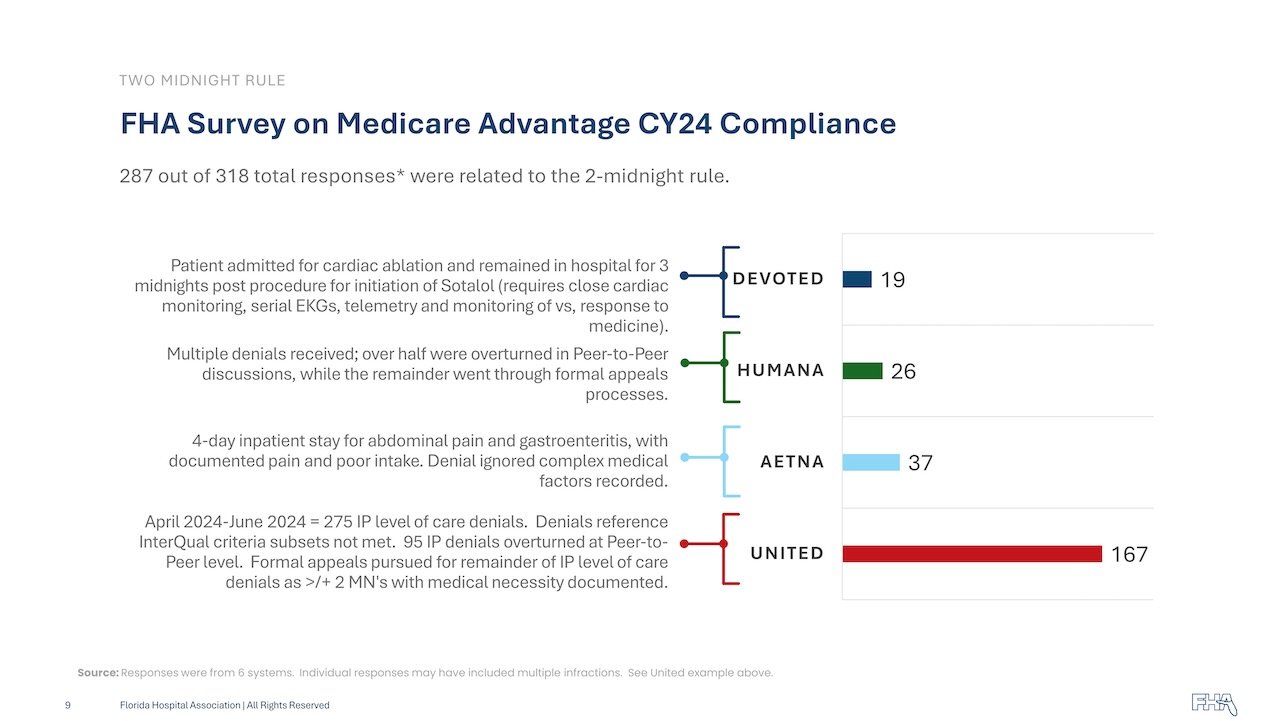
In a release announcing the change, Blessing said some of the reasons providers have cited for making these changes include patient care being delayed due to some Medicare Advantage plans’ pre-authorization process, denial rates and inability to approve needed care. Blessing said some plans apply more stringent medical necessity criteria than traditional Medicare.
Related Articles: Medicare Advantage Updates
-

Aetna, Elevance, Cigna cut some Medicare Advantage broker payments
Payers are taking drastic actions to improve Medicare Advantage margins…and so should Providers.
In an Oct. 31 statement, the National Association of Benefit and Insurance Professionals, which represents brokers, said the rising drug costs and star rating declines have led some insurers to take "drastic action."
-

Hospitals sick of fighting for Medicare Advantage dollars
Hospitals are the most vulnerable provider to rising administrative and financial MA burdens, "given growing risks to reimbursement from MA plans relative to traditional Medicare, as well as the payment risk and higher complexity around prior authorization requirements," according to a recent report from S&P Global. "We also see future risks to providers if at some point CMS addresses the MA program's higher-than-expected spending."
-

Former payer exec: Older adults should avoid Medicare Advantage in 2025
This article highlights the "...significant changes for many older adults and health plans across the country, including shifts in plan quality, increased contract disputes, and market exits from some large carriers."
"If Medicare Advantage provides significant benefits and is a true financial necessity, then that’s the path you should take. However, if you can afford to wait, it may be wise to sit this year out and observe how things unfold."
-

Medicare Advantage's growth a bad omen for hospitals, S&P Global warns
The upward trajectory of Medicare Advantage (MA) enrollment is likely to become an issue for hospitals and other healthcare providers forced to contend with plans’ prior authorization requirements and other reimbursement headwinds, S&P Global warned in a recent report.
-

27 health systems dropping Medicare Advantage plans | 2024
In January, the Healthcare Financial Management Association released a survey of 135 health system CFOs, which found that 16% of systems are planning to stop accepting one or more MA plans in the next two years. Another 45% said they are considering the same but have not made a final decision. The report also found that 62% of CFOs believe collecting from MA is "significantly more difficult" than it was two years ago.